Prior to
moving to the Durango, Colorado area, I had been enrolled in what is called the
Choice Program, which provides military veterans, as well as their dependents,
to obtain care from community resources that are not provided through the VA
system. This is the system I used to receive services such as rheumatology,
gastroenterology, and dermatology. For the most part, this system helped to
provide me with the resources I require to tend to my health needs. Sure, the
physicians and specialists could have just as well been military doctors, as I
received the same quality of care from them...and that is not saying much,
considering my previous experience with military doctors, but I digress.

When I had
my initial appointment with my new primary care provider, I was told something
that just came across as blatantly wrong. See, my doctor told me that my only
options to see these types of specialists would be to drive nearly 4 hours each
way to the large VA facility in Albuquerque, which is insane to suggest, or not
see any specialists. Sure, they have a courtesy shuttle van that takes patients
to the larger facility, but you must plan your day around the appointments of
others, so you would either leave early, or must stay late, depending on the
schedule for that day. The other option just was not feasible either, as I have
a family history of colon and bone cancer, as well as having been diagnosed
with a myriad of chronic pain conditions.
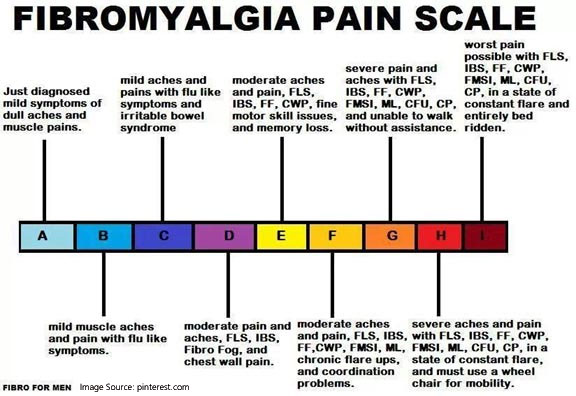 |
| I live at a Level E on a daily basis, just for reference |
You know
the saying “if it sounds too good to be true, it probably is?” Well, that is
applicable to my situation, but rather replace “good” with “wrong” and you see
where I am going with this, right? Well, when I met with the social worker at
my local VA clinic, she repeated the same incorrect information regarding the
Choice Program. She told me that, while there are services in town, such as
support groups, there is little in the way of community resources that address
symptoms. I can’t really go to a support group for my colonoscopy or endoscopy
now, can I?

My social
worker also told me that I am my own advocate for my health, which is a phrase
that she might be wishing she didn’t say. See, I thought that the information I
was provided by not just one, but two medical professionals at my local VA
clinic, sounded incorrect. Just in case though, I called the Choice Program
directly, and boy, am I glad. The representative that I spoke with was just as
befuddled by what I was told as I was when I heard it. It helped to put my mind
at ease, knowing that I was correct about this program, as well as the fact
that I would (hopefully) be able to see a provider here in the community, as my
symptoms have increased since my last visit to the shoddy rheumatologist who
reprimanded me for crying out in pain when he took a biopsy from my thigh at
5:30 in the morning, before I was fully numb. But again, I digress and that,
along with the other numerous experiences I have had with military health
officials and those covered by the Choice Program.

So, here is
my conundrum. Yes, I am my strongest advocate for both my mental and physical
health. The soonest they could schedule me with a mental health professional
(to address my depression, anxiety, PTSD, and MST) is the end of February, and
even then, it would be only via tele-health. That falls outside of the 30 days
or 30-mile rule that applies to the Choice Program (maybe not the distance, but
certainly the time-frame). In the past, I have conveniently fallen through the
VA health cracks, as it had taken me 18 months to even get an appointment with
a rheumatologist, as the original request somehow got lost. I know that I am in
the right and have a whole organization and website that provides me with the
answers to help to support my position. I know that I am most likely not the
only veteran in the area who has been fed this lie. However, I may be the only
one to raise a little hell over the incorrect information that could have
potentially affected the lives of a significant number of veterans living in
the area.

I have been
known to let my emotions get the best of me, particularly when I know that I am
in the right. This isn’t just relegated to my health, but also where we used to
live, I have been physically threatened when I spoke up for the poor treatment
of the dogs I would witness running in the street. As if it were my fault that
I recognized this behavior as wrong and dangerous. I am not kidding. I wish I
were. So, I need to come up with a game plan of sorts, as I know that I need to
go into the clinic and let them know that they are wrong, that I qualify to see
community providers that honor the Choice Program in the area. I know that
other veterans have experienced this same type of treatment. The sooner the
better, but, dude, I am not looking forward to it. I just need to keep my cool,
and remember why I am doing this...for the health of not only myself, but the
countless veterans who have received the same misinformation. Sadly, I know
that this not only applies to my local clinic, but the Portland, Oregon one
too, as that is who contacted me to set up my appointment for the tele-health
mental health sessions...I was told that since they can provide me with the
tele-health services, then I don’t qualify for community care. Well, that is
not true either.



